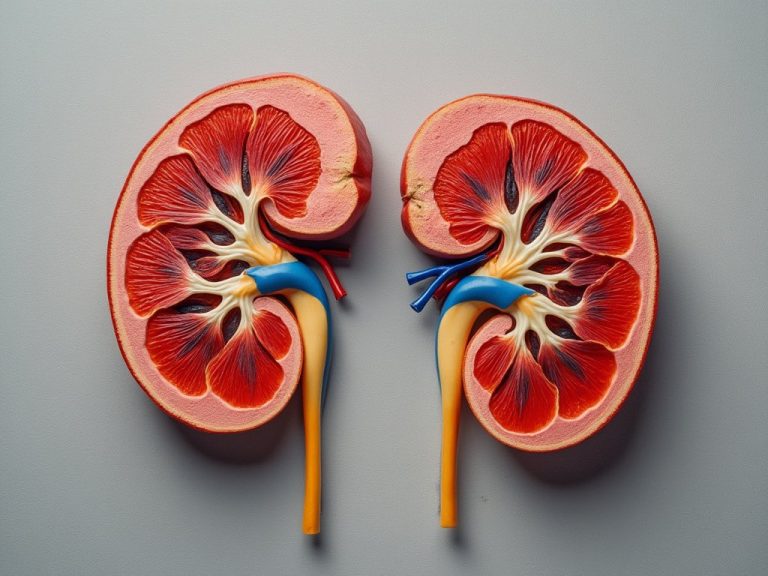
Your kidney is part of a well-designed filtering system in your body. They remove toxins, waste, and extra fluids from your blood through urine. But if your kidneys get injured or damaged, they can’t filter out waste like they’re supposed to. Certain health conditions — such as diabetes and high blood pressure — and several medications can cause this type of damage.
Key takeaways:
- Certain medications, called nephrotoxic medications, can damage your kidneys. This makes it harder for your kidneys to filter waste and other substances from your bloodstream.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, and angiotensin-converting enzyme (ACE) inhibitors have all been linked to kidney problems. Certain medications given in hospital settings, such as iodinated radiocontrast, vancomycin, and aminoglycoside antibiotics, can also hurt the kidneys.
- These aren’t the only medications that are potentially harmful to your kidneys. Talk to a healthcare professional to learn more about how your medications might affect your kidney’s health.
Highlighted below are the top 10 drugs that have been linked to kidney damage. But this doesn’t include everything, so talk to your healthcare professional (HCP) about your full medication list. They can tell you how each medicine might affect your kidney’s health.
1. NSAIDs, like ibuprofen
Nonsteroidal anti-inflammatory drugs (NSAIDs) are popular remedies for pain and fever. And they’re widely used to treat a host of health conditions, such as rheumatoid arthritis, menstrual pain, and inflammation.
Some common NSAIDs are:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve, Naprosyn)
- Meloxicam (Mobic)
- Diclofenac (Cambia)
While NSAIDs such as ibuprofen are generally well-tolerated, taking them does pose some risks. These medications can reduce blood flow through the kidneys, which can contribute to kidney damage or failure. People with heart failure, liver disease, or existing kidney problems are at a higher risk of experiencing new or worsening kidney problems from NSAIDs.
In general, it’s best to take NSAIDs sparingly, at their lowest effective dose, and for the shortest period possible. Occasional doses of NSAIDs taken in recommended amounts are much less likely to cause kidney damage.
2. Diuretics, like hydrochlorothiazide
Diuretics, or water pills, treat health conditions such as high blood pressure and heart failure. Popular diuretics include:
- Hydrochlorothiazide
- Furosemide (Lasix)
- Spironolactone (Aldactone)
- Triamterene (Dyrenium)
These diuretics are typically well-tolerated but, as with all medications, they can cause side effects. One potential diuretic side effect is acute kidney injury, especially in older adults. This is likely because diuretics lower blood volume, which disrupts the filtration process. But diuretics, especially in recommended doses, are not always bad for your kidneys. Kidney damage is more likely with higher doses of diuretics.
3. ACE inhibitors, like lisinopril
Angiotensin-converting enzyme (ACE) inhibitors can be good and bad for your kidneys. These medications are easily identifiable because they end in “-pril,” such as:
- Lisinopril (Zestril)
- Benazepril (Lotensin)
- Enalapril (Vasotec)
- Ramipril (Altace)
ACE inhibitors are go-to medications for managing high blood pressure and heart failure. And in these conditions, they can protect the kidneys. However ACE inhibitors are cleared out of the body through the kidneys, so they also carry a risk of causing kidney injury.
You’re more likely to experience kidney problems related to an ACE inhibitor if you’re dehydrated or taking other nephrotoxic drugs. In either case, you will likely start on a lower dose. Your HCP may also recommend that you come in for routine blood tests to monitor your kidney health over time.
4. Iodinated radiocontrast
Iodinated radiocontrast refers to the contrast dyes used during radiographic testing, such as a CT scan. The dyes make it easier to detect any abnormalities in your organs and blood vessels during the scan.
The downside is that iodinated radiocontrast agents can lead to kidney injury. This type of kidney injury usually appears within 24 to 48 hours of receiving the contrast. The risk factors include having existing chronic kidney disease, having low blood volume, or taking other nephrotoxic drugs.
For people who are at risk of kidney injury from radiocontrast dyes, an HCP will often lower the amount that is used during a test.
5. Vancomycin
Vancomycin is an antibiotic used to treat infections caused by specific bacteria — like methicillin-resistant Staphylococcus aureus (MRSA). It’s frequently used in the hospital when someone has a serious infection.
Kidney damage from vancomycin usually happens within 17 days of beginning treatment with the medication. And kidney function usually improves after treatment is stopped. Pharmacists and prescribers in the hospital work together to closely monitor you and your vancomycin dose every time it’s administered.
6. Aminoglycoside antibiotics, like gentamicin
Aminoglycoside antibiotics, when given as an IV infusion, are known to cause kidney injury. People with chronic kidney disease, who are dehydrated, or who have been taking these antibiotics for longer than 10 days are at higher risk for kidney injury.
Common IV aminoglycoside antibiotics include:
- Gentamicin
- Tobramycin
- Streptomycin
These medications are typically only used in hospital settings, which allows for close monitoring during treatment. An HCP may adjust a person’s dose to be less harmful to their kidneys depending on their medical history and treatment response.
7. HIV medications, like Truvada
Certain HIV medications have been linked to kidney damage. Tenofovir disoproxil fumarate (Viread) — on its own and in combination with products like Truvada and Stribild — can cause acute kidney injury in certain situations. The same goes for atazanavir (Reyataz).
It’s important that anyone planning to take these medications should first be screened for kidney problems. People with existing kidney problems may need to take a lower dose to be safe.
Not all HIV medications carry this risk to the same extent. For instance, the newer formulation of tenofovir, tenofovir alafenamide (Vemlidy), is less likely to cause kidney damage. This is also true for tenofovir alafenamide combination products, such as Descovy and Biktarvy.
8. Other antiviral medications
Other antiviral medications, such as acyclovir (Zovirax) and ganciclovir, can also cause kidney injury. These medications can produce crystals that don’t dissolve in urine. These crystals can cause blockages in the kidney’s filtration system. This side effect is more likely to affect people who are dehydrated or have existing kidney disease.
Foscarnet is another nephrotoxic medication that treats viral infections. It’s not a commonly prescribed medication and it can cause kidney damage rather easily. So, if you need it, your HCP will closely track your kidney function.
9. Zoledronic acid
Zoledronic acid (Reclast) belongs to a group of medications called bisphosphonates. These are used to treat osteoporosis. Kidney damage is a rare but serious side effect associated with zoledronic acid. The FDA issued a formal warning regarding this risk.
In general, Reclast shouldn’t be given to people with abnormal kidney function or preexisting kidney damage. This is also true for Zometa, another version of zoledronic acid used to treat high calcium levels that can occur with certain types of cancer.
10. Calcineurin inhibitors, like tacrolimus
Calcineurin inhibitors, such as cyclosporine modified (Neoral) and tacrolimus (Prograf), are immunosuppressants commonly prescribed to people who have had an organ transplant. These medications have the potential to cause kidney damage.
The benefits of these life-saving medications often outweigh the potential risk of kidney damage, but it’s still good to keep in mind. The risk of kidney damage related to cyclosporine or tacrolimus is worse with higher doses and in people who are already at risk of kidney damage. If you take either of these medications, your HCP will likely monitor your kidneys.
When should you see a healthcare professional about suspected kidney problems from your medication?
It’s not always easy to tell if you have kidney damage. You might not experience any symptoms. Your HCP may only notice signs of it after running certain lab tests.
However, if you notice any of these symptoms, talk to your HCP right away:
- Blood or foam in the urine
- Dark-colored urine
- A noticeable change in urinary frequency
- Lower back or flank pain
- Decreased or difficulty urinating
If you report any of these side effects, your HCP will likely order lab tests to evaluate your kidney health. Based on these results and what medications you are taking, you may need to stop or pause treatment. In some cases, you may be able to switch to a medication that is safer for your kidneys.
By Hindu Rao, PharmD, APh, BCACP, a clinical assistant professor of pharmacy practice at Chapman University School of Pharmacy and a clinical pharmacist at Providence Medical Foundation. She specializes in chronic disease management and has her board certification in ambulatory care.