A new study has revealed that antimicrobial resistance (AMR) continues to spread in the environment despite a notable reduction in antibiotic prescriptions — raising fresh concerns about the complexity of combating one of the world’s deadliest public health threats.
The research, led by scientists at the University of Bath and published in the Journal of Global Antimicrobial Resistance, was made available on Thursday in Abuja.
The study cautioned that simply reducing antibiotic usage may not be sufficient to curb the rising threat of AMR, which the World Health Organization (WHO) estimates is linked to over five million deaths annually.
Researchers called for a broader, multi-pronged strategy—including environmental management, improved sanitation, and stricter controls on pharmaceutical waste—alongside continued efforts to promote responsible antibiotic use in both humans and animals.
The study was based on wastewater analysis, conducted in partnership with Wessex Water, using samples collected over a two-year period from four wastewater treatment plants in southwest England. Scientists monitored antibiotic concentrations and AMR gene presence and compared the data with both pre-pandemic findings and local prescription records.
Prof. Barbara Kasprzyk-Hordern, Director of the Centre of Excellence in Water-Based Early-Warning Systems for Health Protection (CWBE), led the research and shared key insights.
She explained that although antibiotic prescriptions dropped between 2017 and 2019—and the presence of antibiotics in wastewater declined—resistance genes remained at high levels.
“There was a temporary reduction in AMR genes during the 2020 COVID-19 lockdowns, likely due to decreased human activity and interaction,” Kasprzyk-Hordern said. “But both antibiotic use and AMR gene prevalence rebounded quickly post-lockdown.”
She emphasized that this trend points to environmental transmission as a major contributor to the spread of resistance.
“It’s not just about how many antibiotics we consume. Once resistance genes enter the environment, they can spread rapidly between bacteria,” she added.
The researchers advocated for a One Health approach that integrates human, animal, and environmental health measures. Their ongoing work at CWBE supports this vision through a newly established “living lab” to monitor pathogens and chemical exposure and link these findings to health outcomes.
Dr. Like Xu, the study’s first author, highlighted the value of wastewater-based epidemiology as a cost-effective and powerful tool in tracking resistance trends.
“It enables real-time data collection that can guide public health responses and policy decisions,” Xu stated.
The findings underscore the urgent need for global, cross-sectoral collaboration to halt the silent spread of AMR—especially beyond clinical settings and farms, into water systems that link entire communities.
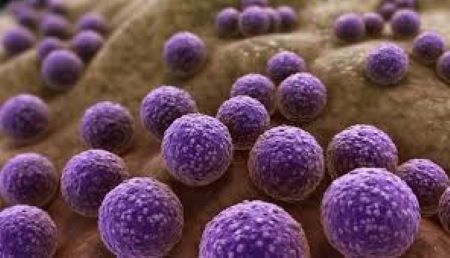
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites evolve to resist medications, rendering infections more difficult—and sometimes impossible—to treat.
It leads to longer illnesses, higher treatment costs, and increased mortality.
In Nigeria alone, AMR was responsible for over 263,000 deaths in 2019, surpassing fatalities from both malaria and tuberculosis.
Key drivers of AMR include:
- Overuse and misuse of antibiotics in human and animal care
- Poor infection control practices
- Weak enforcement of regulations
- Self-medication and public misuse of antimicrobial drugs
Experts warn that tackling AMR effectively will require strong engagement from all sectors, particularly the private health sector, which delivers more than 60% of healthcare services in Nigeria.