For a condition that affects up to 10% of reproductive-age women worldwide, polycystic ovary syndrome (PCOS) remains mysterious. It’s a leading cause of female infertility and often boosts the risk of metabolic problems such as type 2 diabetes. It’s also highly heritable: The sister of an affected woman has at least a 20% chance of developing it herself, and the risk for identical twins is even higher.
Yet although there are many symptoms of PCOS—including lack of ovulation, ovarian cysts, and excess hair growth on the face and body—no one seems to know how it starts. Is it driven by genes? A woman’s environment? Increasingly, researchers are considering a third category: life in the womb. There’s more and more evidence that when a mom has PCOS, her female baby-to-be experiences shifts in hormones while in utero that can cause the syndrome many years later. In particular, several studies in pregnant animals have shown that exposing them to hormones like testosterone, which women with PCOS produce at higher levels, leads to lack of ovulation and other PCOS-like symptoms in female offspring.
Now, a paper published today in Nature Medicine builds on that evidence. Based primarily on findings in mice, it suggests that interactions between a hormone produced by the ovaries and a set of neurons in mom’s brain can have a cascade effect, disrupting enzymes in the placenta and ultimately causing PCOS-like symptoms in her offspring.
Still, it’s not clear whether the hormonal effects recorded in the rodents happen in pregnant women. And for now, the work doesn’t offer an immediate avenue to preventing PCOS in utero.
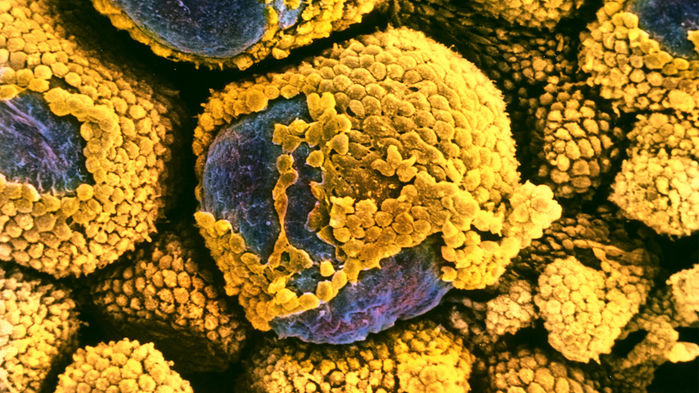
Seeking insight into the condition, Paolo Giacobini, a neuroendocrinologist at the University of Lille in France, focused on antimüllerian hormone (AMH), which is produced by small follicles on the ovary. Women with PCOS have an excess of those follicles, and therefore they make more AMH. Giacobini’s group had previously found that AMH could act on a set of neurons in the brain, which then triggers the release of luteinizing hormone (LH) by part of the pituitary gland. In healthy women, a surge in LH triggers ovulation, but in women with PCOS, the hormone is constantly at a high level, which in turn suppresses ovulation and boosts the release of testosterone—two hallmarks of the syndrome.
Giacobini and colleagues initially gathered blood samples from four groups of pregnant women in their second trimester: obese and nonobese women without PCOS, and obese and nonobese women with PCOS. Normally, AMH levels fall in pregnancy because the ovaries aren’t active. In the lean PCOS group, AMH levels were about two to three times as high as in the other three groups. It’s not known why the obese women with PCOS didn’t have higher levels, too.
Giacobini’s group then turned to mice. They injected some pregnant rodents with AMH late in pregnancy to mimic the high levels of the hormone in the women they’d studied. The female offspring developed symptoms resembling PCOS, such as rare ovulation and high testosterone levels. Additional studies suggested excess testosterone from the mothers was crossing the placenta and affecting the fetuses. This happened, the group theorized, because AMH damped down levels of aromatase, an enzyme in the placenta that usually converts testosterone to a form of estrogen. With aromatase activity curtailed, extra testosterone snuck through and bathed the mouse fetuses in a PCOS-conducive environment.
Although PCOS researchers agree the mouse work is strong, they’re mixed on whether it could be true of PCOS in women. “Whether all these things happen in humans, we don’t know,” says Jeffrey Chang, a reproductive endocrinologist at the University of California (UC), San Diego. Human placentas contain a lot more aromatase than mouse placentas do, for example, suggesting it would be harder to overwhelm aromatase activity in people. “You would have to just have gobs and gobs of testosterone being produced” for that to happen, even if some of the placenta’s aromatase was blunted, says Jerome Strauss, a reproductive endocrinologist at Virginia Commonwealth University in Richmond. The model’s “transportability to human biology is very difficult,” he says.
Still, one theme that makes the work intriguing to some is that it focused on lean animals and women with PCOS, who are a sizable subgroup of those with the syndrome. Previous work on the fetal environment had focused on metabolic abnormalities that are much more obvious in overweight women with PCOS, who have an increased risk of developing diabetes in pregnancy. This shows that it’s possible that “even a lean person can program” the fetus, says Daniel Dumesic, a reproductive endocrinologist at UC Los Angeles. That finding is supported, he says, by the blood tests that showed high AMH levels in lean pregnant women with PCOS.
Ultimately, though, most agree that testosterone, which AMH also boosts via a cascade, is probably a key culprit behind the malady. This new work is “another brick in the wall” suggesting that hormones such as testosterone—perhaps fueled by extra AMH—could be paving the way for PCOS in fetuses, says Sue Moenter, a physiologist at the University of Michigan in Ann Arbor. Giacobini and others are studying whether interventions to head off the syndrome might work at different ages in the mouse—a strategy much more likely to lead somewhere than one given in pregnancy, where modulating hormones in a developing fetus, and pregnant woman, can be riskier. Science